Losing a tooth is about more than just the gap it leaves in your smile. A hidden process begins almost immediately in your jawbone. The specific part that once anchored your tooth, known as the alveolar ridge, starts to shrink and recede because it no longer has a job to do. This can change your facial structure and make it difficult, or even impossible, to get a dental implant later on. Fortunately, modern dentistry has a powerful solution. Using advanced bone grafting techniques and protective membranes, we can rebuild this essential foundation, creating the perfect, stable base for a future implant. This guide will explain exactly how these procedures work, demystifying the process and showing you how we can preserve your jaw for a lifetime of healthy smiles.
Bone grafts and membranes have revolutionized the field of dentistry, enabling remarkable advancements in extraction procedures. In this blog post, we will explore the state-of-the-art techniques and innovations in bone grafting and membrane usage, highlighting their benefits, applications, and future prospects.
What Are Dental Bone Grafts and Membranes?
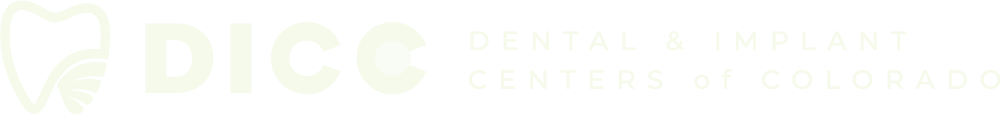
Bone grafting is a technique used to replace or stimulate the growth of missing bone. It involves the transplantation of bone or bone-like materials to the site where bone regeneration is desired. By providing a scaffold for new bone formation, bone grafts facilitate the healing process and enable successful dental procedures. Membranes, on the other hand, play a crucial role in guided tissue regeneration (GTR) procedures. They act as barriers, preventing unwanted soft tissue infiltration into the graft site while allowing for the migration and proliferation of bone-forming cells. Membranes can be classified into resorbable and non-resorbable types, depending on their degradation characteristics. Different types of bone grafts are available for use in dental procedures. Autografts involve using the patient’s own bone, harvested from another site in the body. Allografts use bone from a donor, either from a cadaver or a tissue bank. Xenografts utilize bone derived from animal sources, such as bovine or porcine. Synthetic graft materials, such as hydroxyapatite or calcium phosphate, offer alternative options for patients with specific needs. Before performing a bone grafting procedure, assessing the quality of the patient’s existing bone is essential. This evaluation helps determine the appropriate type and amount of graft material required for optimal outcomes. Diagnostic imaging, such as cone-beam computed tomography (CBCT), aids in the assessment process. Read more: Bone Grafting 101: What It Is And When It Is Necessary
Types of Bone Grafts
When your dentist recommends a bone graft, it’s natural to have questions about where the material comes from. The goal is always the same: to provide a stable foundation for your jaw, often in preparation for a dental implant. However, there are several different types of grafting materials, each with its own set of benefits. Understanding these options can help you feel more confident and prepared for your procedure. The right choice depends on your specific health needs, the extent of bone loss, and your personal preferences. At Dental & Implant Centers of Colorado, we walk you through each option to find the perfect fit for your treatment plan.
Autograft: The Gold Standard
An autograft is often called the “gold standard” in bone grafting, and for good reason. This type of graft uses your own bone, typically harvested from another area of your body like the chin, jaw, or hip. Because the material is your own, it contains living bone cells and growth factors that actively encourage new bone to form. This also means there is virtually no risk of your body rejecting the graft material, leading to highly predictable and successful outcomes. The main consideration with an autograft is that it requires a second surgical site to collect the bone, which means a slightly longer recovery process. However, for many patients, the reliability and effectiveness make it the best possible choice for rebuilding a strong, healthy jaw.
Allograft: A Donor-Based Option
An allograft offers a fantastic alternative that avoids the need for a second surgical site. This type of graft uses bone from a human donor that has been carefully screened, sterilized, and processed by a certified tissue bank to ensure it’s completely safe for use. The primary advantage is convenience—you only have one area that needs to heal. The donor bone acts as a scaffold, or a framework, that your own body uses to build new bone tissue over time. While the results can be slightly less predictable than with an autograft because it doesn’t contain living cells, allografts have a long track record of success in dental procedures and are an excellent option for many patients seeking to restore their jaw structure.
Xenograft: An Animal-Sourced Scaffold
A xenograft is another common and highly effective option that uses bone derived from an animal source, most often a cow (bovine). The mineral structure of this bone is very similar to human bone, making it an ideal scaffold for your body to build upon. The xenograft material is put through a rigorous purification process to remove all organic material, leaving only the mineral framework behind. This framework encourages your own bone cells to grow into the area and regenerate the jaw. One of the unique benefits of a xenograft is that it resorbs, or breaks down, very slowly, providing long-lasting support as your new bone develops. It’s a reliable material used in many of our dental services to ensure a solid foundation for future treatments.
Synthetic Grafts: Lab-Created Alternatives
For patients who prefer to avoid human or animal-derived materials, synthetic grafts are an excellent, lab-created alternative. These grafts are typically made from biocompatible materials like calcium phosphates, which mimic the composition of natural bone. Just like other graft types, synthetic materials act as a scaffold, creating a space where your body can generate new bone tissue. They are completely sterile and carry no risk of disease transmission. While some studies suggest they may not integrate as quickly as other options, advancements in material science are constantly improving their effectiveness. Synthetic grafts provide a safe, predictable, and ethical choice for rebuilding bone and preparing your smile for what’s next, like a beautiful new dental implant.
Understanding Dental Membranes
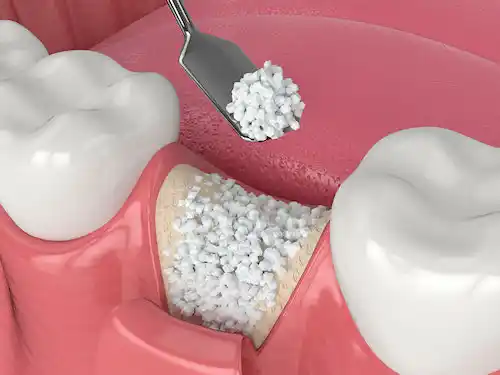
After a bone graft is placed, the work isn’t quite done. The site needs to be protected to ensure that the right kind of cells—bone cells—are the only ones that grow in that space. Soft tissue, like your gums, tends to heal much faster than bone. Without a barrier, gum tissue could grow into the graft area and interfere with proper bone regeneration. This is where dental membranes come in. These thin, biocompatible sheets are placed over the bone graft to act as a protective shield, guiding the healing process and ensuring the best possible outcome for your procedure.
Resorbable vs. Non-Resorbable Membranes
Dental membranes generally fall into two categories: resorbable and non-resorbable. Resorbable membranes are designed to naturally and safely dissolve on their own over a period of weeks or months as your body heals. This is a huge plus for patients, as it eliminates the need for a second surgery to have the membrane removed. They are typically made from materials like collagen and are quite flexible and easy for your surgeon to work with. Non-resorbable membranes, on the other hand, are made from materials that do not break down in the body. They provide a more rigid and long-lasting barrier, which can be necessary for larger defects. However, they do require a follow-up procedure for removal once the bone has fully healed.
The Role of Collagen Sponges
In many extraction and grafting procedures, you might also hear about the use of collagen sponges or plugs. These are small, sponge-like pieces of purified collagen that are placed directly into the empty tooth socket or graft site. They play a few very important roles in the healing process. First, they help stabilize the blood clot, which is the foundation for all new tissue growth. Second, they protect the delicate wound from food particles and bacteria, reducing the risk of infection. Finally, they provide a soft scaffold that encourages the formation of new, healthy gum tissue over the site. Our expert team often uses these to ensure a smooth and comfortable healing experience for our patients.
Understanding the Alveolar Ridge: Your Jaw’s Foundation
Before we can appreciate why procedures like bone grafting are so important, it helps to understand the structure they are designed to support. Think of your jawbone as the foundation of your smile. The specific part of the jaw that anchors your teeth is called the alveolar ridge. It’s a crest of bone on your upper (maxilla) and lower (mandible) jaws that contains the sockets for your teeth. This ridge creates the curved dental arch that gives your mouth its shape. When this foundation is strong and healthy, it provides the stable base needed for your natural teeth and is absolutely essential for the long-term success of restorative solutions like dental implants.
The Anatomy and Composition of Your Jawbone
The alveolar ridge isn’t just a static piece of bone; it’s a dynamic, living tissue. Composed of a mix of inorganic minerals like calcium and organic materials like collagen, this bone is in a constant state of remodeling. Specialized cells are always at work: osteoblasts act as the construction crew, building new bone, while osteoclasts are the demolition team, breaking down old bone. This continuous cycle allows your jaw to adapt to the pressures of chewing and other forces. Understanding this process is key to grasping why the bone can shrink after a tooth is lost and, more importantly, how it can be successfully rebuilt to support your oral health.
The Critical Functions of the Alveolar Ridge
The alveolar ridge does more than just hold your teeth in place. It plays a surprisingly significant role in several everyday functions that we often take for granted. For instance, it’s crucial for clear speech. When you form sounds like “t,” “d,” or “s,” your tongue makes contact with the alveolar ridge just behind your upper front teeth. It’s also vital for effective chewing, as it helps contain food while you break it down. When a tooth is lost and the ridge begins to change shape, it can impact not only your smile’s appearance but also these fundamental aspects of your daily life.
Tooth Extraction and Jawbone Health
Losing a tooth sets off a chain reaction in your jaw. Without the tooth root to stimulate it, the alveolar ridge no longer has a job to do in that area, and the body begins to resorb the bone. This process is a natural response, but it can create significant challenges for future dental work. The jawbone can shrink surprisingly quickly, which is why addressing a missing tooth promptly is so important. Maintaining that bone volume is the key to preserving your facial structure and keeping all your options open for tooth replacement, ensuring you can choose the best solution for your health and lifestyle.
What Happens to the Bone After a Tooth is Pulled?
The rate of bone loss after an extraction can be quite dramatic. Research shows that without any intervention, the alveolar ridge can lose an average of 3.8 millimeters in width and 1.24 millimeters in height within the first six months alone. This resorption process continues over time, leading to a narrower and shorter ridge. This not only affects the stability of neighboring teeth but can also make it impossible to place a dental implant later without an additional bone grafting procedure. Acting quickly helps preserve the jaw’s natural shape and strength, making future restorative services much more straightforward and predictable.
The Natural Healing Process Explained
After a tooth is extracted, your body immediately kicks off a sophisticated, three-stage healing process. The first few days are defined by the inflammation stage, where a blood clot forms in the socket to protect the underlying bone. About two weeks later, the new bone formation stage begins as your body starts building a soft, new bony matrix. Finally, the bone remodeling phase kicks in, which can take several months or even longer. During this last stage, the new bone matures and hardens. While this natural process is amazing, it doesn’t prevent the ridge from shrinking, which is why your dentist may recommend specific techniques to preserve it.
Factors That Can Complicate Healing
While the body is designed to heal, several factors can interfere with the process after a tooth extraction. Pre-existing conditions like gum disease, infections, or systemic issues such as diabetes can slow down recovery. Lifestyle choices, particularly smoking, can significantly restrict blood flow to the area and impair healing. Even the extraction itself, if traumatic, can affect the outcome. This is why having an experienced professional is so important. The expert team at DICC can assess your individual risk factors and create a plan to manage them, ensuring your recovery is as smooth and successful as possible.
How Modern Bone Grafting Technology is Changing Dentistry
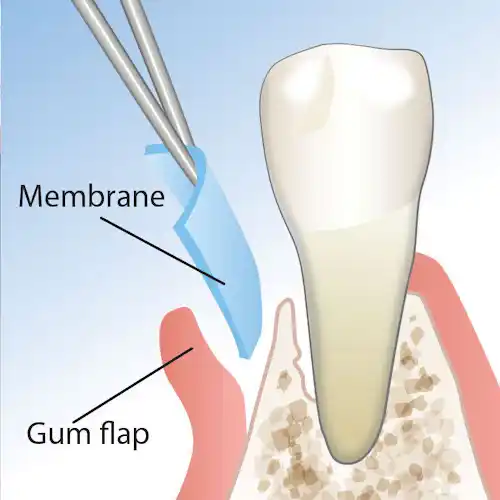
Socket preservation is a technique aimed at minimizing bone loss following tooth extraction. The process involves placing a bone graft material directly into the extraction socket. This approach promotes the preservation of the natural bone contour and prevents subsequent bone resorption, providing a solid foundation for future implant placement. Ridge augmentation is another area that has witnessed significant advancements. It involves the use of bone grafts to augment and reconstruct the alveolar ridge, restoring its height and width. This technique is crucial when the ridge lacks sufficient bone volume for successful implant placement. Innovative grafting materials and techniques, such as particulate grafts, block grafts, and split-crest procedures, have improved the predictability and success rates of ridge augmentation procedures. Sinus lifts, or maxillary sinus floor augmentation, are commonly performed to increase the bone height in the posterior maxilla for dental implant placement. The procedure involves lifting the sinus membrane and filling the space below it with bone graft material. Advancements in sinus lift techniques, such as the minimally invasive lateral window approach and crestal approach using osteotomes, have made the procedure more predictable and less invasive. In recent years, navigated bone grafting techniques have emerged as a cutting-edge approach. Computer-guided systems enable precise preoperative planning and real-time intraoperative guidance, enhancing the accuracy and efficiency of bone graft placement. The use of navigation systems minimizes surgical errors, reduces patient discomfort, and facilitates quicker healing.
Atraumatic Extractions: The First Step in Preservation
The entire process of preserving your jawbone starts with a technique called “atraumatic extraction.” This simply means removing a tooth as gently as possible to minimize damage to the surrounding bone and gums. Why is this gentle approach so critical? When a tooth is removed, the jawbone that once supported it begins to shrink, a process called resorption. A traditional, more forceful extraction can speed up this bone loss, making it more challenging to place a dental implant down the road. At Dental & Implant Centers of Colorado, our specialists prioritize this technique to preserve as much of your natural bone as possible, creating a stronger foundation for your future restoration and setting you up for long-term success.
How Dental Membranes Help Your Body Heal
Guided tissue regeneration (GTR) is a technique that uses membranes to create a protected space for the regeneration of periodontal tissues. By placing a barrier membrane between the soft tissues and the defect site, GTR prevents the migration of epithelial cells and allows the proliferation of periodontal ligament cells and bone-forming cells, promoting the regeneration of periodontal tissues.
What’s Next for Bone and Tissue Regeneration?
Advancements in biomaterials have the potential to revolutionize bone grafting outcomes. Researchers are exploring the use of growth factors, bioactive molecules, and tissue-engineered constructs to enhance bone regeneration. The integration of these biomaterials into bone grafting procedures can accelerate healing, promote tissue integration, and improve overall clinical outcomes. Membrane technology is also advancing rapidly. New membrane designs and materials are being developed to optimize the barrier properties, degradation rates, and handling characteristics. Resorbable membranes with controlled release properties, customizable shapes, and improved tissue integration capabilities are expected to enhance the success rates of guided bone regeneration procedures. Tissue engineering and regenerative approaches hold great promise in the field of bone grafting. Scientists are working on developing techniques to cultivate patient-specific bone tissue in the lab, which can be subsequently transplanted into the defect site. These regenerative therapies aim to provide a renewable and biocompatible source of bone grafts, minimizing the need for donor materials. Virtual planning and guided surgeries are becoming increasingly popular in bone grafting procedures. Through the use of advanced imaging techniques, such as CBCT and 3D models, virtual treatment planning enables precise preoperative analysis, accurate graft placement, and improved clinical outcomes. Additionally, computer-guided implant surgeries and robotic-assisted procedures are being explored to enhance the precision and efficiency of bone grafting.
Had a Tooth Pulled? Why an Implant Should Be Your Next Step
Top Reasons to Choose a Dental Implant After Extraction
There are several reasons why you might consider getting dental implants after an extraction:
1. Eat and Speak with Confidence Again
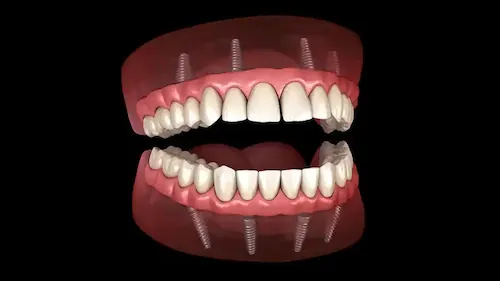
Dental implants provide a functional replacement for the missing tooth. They are designed to mimic the natural tooth root and offer stability and support for biting and chewing. By getting a dental implant, you can regain the ability to eat and speak properly, improving your overall quality of life.
2. Protect Your Jawbone and Facial Structure
When a tooth is extracted, the underlying jawbone can begin to deteriorate over time due to lack of stimulation. Dental implants stimulate the jawbone through the process of osseointegration, where the implant fuses with the bone. This helps preserve the bone structure and prevent further bone loss. Without an implant, the surrounding bone may start to resorb, potentially leading to changes in facial appearance and shifting of neighboring teeth.
3. Keep Your Other Teeth From Shifting
After a tooth extraction, neighboring teeth can gradually shift and move into the empty space, causing misalignment and bite problems. By replacing the extracted tooth with a dental implant, you maintain proper spacing and alignment of your teeth, preventing these issues and preserving the overall integrity of your dental arch.
4. Restore Your Natural-Looking Smile
Missing teeth can have a significant impact on your smile and facial appearance. Dental implants provide a natural-looking and aesthetically pleasing solution for replacing missing teeth. They are custom-made to blend seamlessly with your existing teeth, enhancing your smile and boosting your self-confidence.
5. Invest in a Long-Lasting Solution
Dental implants are known for their durability and longevity. With proper care and maintenance, implants can last for many years or even a lifetime. Compared to other tooth replacement options, such as dentures or bridges, implants offer a more permanent and stable solution.
6. Support Your Overall Oral Health
Dental implants do not require altering or compromising adjacent teeth, as is often the case with dental bridges. By opting for an implant, you can maintain the health and integrity of your remaining natural teeth. Implants are also easy to clean and maintain, just like your natural teeth, promoting good oral hygiene and reducing the risk of dental issues in the future. It’s important to consult with a qualified dental professional who can evaluate your specific case and provide personalized recommendations. They will consider factors such as your overall oral health, bone condition, and treatment goals to determine if dental implants are the best option for you after an extraction.
7. A Highly Successful and Reliable Solution
It’s reassuring to know that dental implants have an outstanding success rate, hovering around 99%. This makes them one of the most reliable solutions in modern dentistry for replacing missing teeth. While failures are uncommon, they can sometimes occur, particularly in the front part of the upper jaw. This is often because the bone in that area is naturally thinner and less dense, which can make it challenging for an implant to integrate securely. This is precisely why a procedure like bone grafting is so crucial. By building up the jawbone, our specialists at Dental & Implant Centers of Colorado create a strong, stable foundation, ensuring your implant has the best possible chance for long-term success and giving you a result you can count on.
Why an Extraction Might Be Needed Before an Implant
In many cases, a dental extraction is necessary before a dental implant can be placed. If a tooth is severely damaged or compromised due to decay, trauma, or periodontal disease, extraction may be the recommended treatment option. After the tooth is extracted, the site is allowed to heal, and then a dental implant can be placed in the same location to restore the missing tooth.
Saving the Socket for a Future Implant
In situations where a tooth extraction is required but immediate implant placement is not feasible, socket preservation techniques may be employed. Socket preservation involves placing bone graft material into the extraction socket immediately after tooth removal. This helps to maintain the volume and contours of the socket, preventing excessive bone loss. The preserved socket provides a more favorable environment for future dental implant placement, ensuring adequate bone support and improving the overall success of the implant procedure.
Building Up the Alveolar Ridge for a Strong Foundation
In cases where the alveolar ridge has experienced bone resorption or lacks sufficient width or height, ridge augmentation procedures may be performed. Ridge augmentation involves adding bone graft material to the deficient ridge area to rebuild or enhance its dimensions. This procedure creates a more suitable foundation for implant placement, ensuring optimal aesthetics and function. Ridge augmentation may be necessary prior to dental implant placement to ensure the long-term success of the implant by providing adequate bone support.
Surgical Approaches to Ridge Augmentation
When it comes to rebuilding your jawbone, your surgeon has a couple of main techniques they can use. The choice really comes down to what will give you the best result for your specific situation. One common method is the “flap” approach, where the gum tissue is gently lifted to give the surgeon a clear view of the area. This allows for precise placement of the bone graft material. Another option is the “flapless” technique, which is a more minimally invasive approach. With this method, the graft is placed through a small opening in the gum, avoiding the need to lift a larger section of tissue. This can often mean less discomfort and a quicker recovery for you. The decision between these two isn’t one-size-fits-all; our specialists carefully evaluate your bone quality and the extent of the bone loss to select the surgical approach that sets your future implant up for success.
Replacing a Failing Tooth with a Secure Implant
Dental extractions may be performed on teeth that are severely damaged, decayed, or non-restorable. In such cases, the failing tooth is extracted, and a dental implant is placed as a replacement. Implants serve as a stable and durable solution for tooth replacement, offering numerous benefits such as improved chewing ability, natural appearance, and preservation of jawbone structure. Dental implants provide a long-term solution for patients who have lost teeth due to various reasons, and they can significantly enhance oral health and quality of life.
How Bone Grafts and Membranes Make Implants Possible
Why Grafts and Membranes Are Key to Implant Success
They play a crucial role in preparing the implant site and ensuring the long-term success of implant procedures. Here’s how they are connected:
Creating Enough Bone for a Stable Implant
Bone grafting techniques are used to augment or regenerate bone in areas where there is insufficient natural bone volume for dental implant placement. By adding bone graft material to the deficient area, bone volume and density can be improved, providing a solid foundation for implant stability. The bone graft acts as a scaffold, promoting new bone growth and integration with the surrounding natural bone. This process enhances the chances of successful implant osseointegration, ensuring the implant remains stable and durable over time.
Using Socket Preservation to Prepare the Site
When a tooth is extracted, the socket that remains can undergo bone resorption and lead to the loss of bone volume. Socket preservation involves placing bone graft material immediately after tooth extraction to maintain the dimensions of the extraction socket. By preserving the socket, bone loss is minimized, and the site is better prepared for subsequent dental implant placement. The bone graft helps retain the natural bone contour, facilitating optimal implant positioning and stability.
How Ridge Augmentation Creates the Perfect Fit
In cases where the alveolar ridge lacks adequate height or width, ridge augmentation techniques are employed to augment the ridge before dental implant placement. Bone grafts are used to rebuild or augment the deficient areas of the ridge, creating a more suitable site for implant placement. Ridge augmentation techniques help establish a proper bone foundation, enabling the implant to be placed in an ideal position for optimal aesthetics and function.
Making Room for Implants with a Sinus Lift
Maxillary sinus lifts, or sinus floor augmentation, are performed when the maxillary sinus is too close to the upper jaw, limiting the available bone height for implant placement in the posterior region. In this procedure, the sinus membrane is lifted, and bone graft material is added to the space created between the sinus floor and the ridge. This creates additional bone volume in the posterior maxilla, allowing for successful implant integration. Sinus lifts are essential in cases where implants are desired in the upper molar and premolar areas.
Guiding New Bone Growth Where You Need It
Membrane techniques are employed in guided tissue regeneration (GTR) procedures to promote the selective growth of bone and connective tissues while preventing the infiltration of unwanted soft tissue cells. Barrier membranes are placed between the bone graft material and the surrounding soft tissues to create a protected space. This space allows bone-forming cells to populate the graft site, leading to the regeneration of bone, which is crucial for the integration and stability of dental implants. In summary, bone graft and membrane techniques are integral to the success of dental implant procedures. They contribute to the preparation and augmentation of the implant site, ensuring sufficient bone volume and density for stable implant placement. These techniques facilitate osseointegration, improve implant stability, and enhance long-term implant success rates. Dental implants do not require altering or compromising adjacent teeth, as is often the case with dental bridges. By opting for an implant, you can maintain the health and integrity of your remaining natural teeth. Implants are also easy to clean and maintain, just like your natural teeth, promoting good oral hygiene and reducing the risk of dental issues in the future. It’s important to consult with a qualified dental professional who can evaluate your specific case and provide personalized recommendations. They will consider factors such as your overall oral health, bone condition, and treatment goals to determine if dental implants are the best option for you after an extraction.
From Extraction to Implant: Understanding the Process
Dental extractions and dental implants are related in the context of replacing missing teeth. Here’s how they are connected:
When an Extraction Is the First Step
In many cases, a dental extraction is necessary before a dental implant can be placed. If a tooth is severely damaged or compromised due to decay, trauma, or periodontal disease, extraction may be the recommended treatment option. After the tooth is extracted, the site is allowed to heal, and then a dental implant can be placed in the same location to restore the missing tooth or teeth.
Protecting the Socket for Your Future Implant
In situations where a tooth extraction is required but immediate implant placement is not feasible, socket preservation techniques may be employed. Socket preservation involves placing bone graft material into the extraction socket immediately after tooth removal. This helps to maintain the volume and contours of the socket, preventing excessive bone loss. The preserved socket provides a more favorable environment for future dental implant placement, ensuring adequate bone support and improving the overall success of the implant procedure.
Timeline for Placing an Implant After Preservation
So, how long do you have to wait after socket preservation? Patience is key here, as your body needs time to heal before an implant can be placed. The timeline really depends on the type of graft material used and how your own body heals, but a typical wait is about 3 to 4 months. This waiting period is essential for the new bone to fully integrate, creating a strong and stable base for your future dental implant. While some people might be ready in as little as 6 weeks, others may need up to 9 months. Your dental specialist will keep a close eye on your progress to pinpoint the ideal time for placement. This careful timing is what ensures your implant has the best support and helps prevent the jawbone shrinkage that can occur after an extraction.
Preparing the Alveolar Ridge for Your Implant
In cases where the alveolar ridge has experienced bone resorption or lacks sufficient width or height, ridge augmentation procedures may be performed. Ridge augmentation involves adding bone graft material to the deficient ridge area to rebuild or enhance its dimensions. This procedure creates a more suitable foundation for implant placement, ensuring optimal aesthetics and function. Ridge augmentation may be necessary prior to dental implant placement to ensure the long-term success of the implant by providing adequate bone support.
Replacing Hopeless Teeth with Lasting Implants
Dental extractions may be performed on teeth that are severely damaged, decayed, or non-restorable. In such cases, the failing tooth is extracted, and a dental implant is placed as a replacement. Implants serve as a stable and durable solution for tooth replacement, offering numerous benefits such as improved chewing ability, natural appearance, and preservation of jawbone structure. Dental implants provide a long-term solution for patients who have lost teeth due to various reasons, and they can significantly enhance oral health and quality of life.
The Alveolar Ridge in Broader Dental Health
The Link Between Periodontal Disease and Bone Loss
It’s easy to think of gum disease as just a problem with your gums, but its effects run much deeper—right down to the bone. Periodontal disease is one of the main reasons people experience alveolar bone loss. When a chronic infection takes hold in your gums, the persistent inflammation starts to break down the very bone that anchors your teeth in place. This isn’t a quick process, but over time, it can cause teeth to become loose and eventually lead to tooth loss. That’s why addressing gum health is a non-negotiable first step in preserving your jawbone and your smile. A holistic approach to dental care focuses on treating the root cause, ensuring your entire mouth is healthy before moving on to restorative solutions like implants.
Other Clinical Considerations
The health of your alveolar ridge impacts more than just whether your teeth stay put. It plays a role in many other areas of dentistry, underscoring its importance for your overall health. For instance, it’s a critical site for bone grafting procedures in children born with a cleft palate. The density of the ridge can also influence how dental infections spread and even determine how effective local anesthesia is during a procedure. In some rare cases, conditions like anodontia, where a person is born without teeth, can prevent the alveolar ridge from developing correctly in the first place. These wide-ranging factors show why having a team of experienced professionals is so important for managing your dental health comprehensively.
Frequently Asked Questions
Is a bone graft absolutely necessary every time a tooth is pulled? Not always, but it’s highly recommended if you’re considering a dental implant in the future. Think of it as proactive care. When a tooth is removed, the jawbone in that area starts to shrink almost immediately. Placing a bone graft right away preserves that foundation, making a future implant procedure much more straightforward and successful. If you wait, you might need a more complex grafting procedure later to rebuild the bone that has been lost.
Does getting a bone graft hurt? This is a very common concern, and the short answer is no, the procedure itself shouldn’t hurt. Your dental specialist will make sure the area is completely numb with local anesthesia before they begin. Afterward, it’s normal to experience some mild soreness and swelling, similar to what you’d feel after an extraction. This discomfort is typically easy to manage with over-the-counter pain relievers and by following the aftercare instructions we provide.
What happens if I don’t get a bone graft and just let the socket heal naturally? Your body will absolutely heal the socket on its own, but it won’t preserve the bone. Without a tooth root or a graft to support it, the alveolar ridge—the part of your jaw that holds teeth—will begin to shrink in both height and width. This can cause neighboring teeth to shift, affect your facial structure over time, and make it much more difficult to place a dental implant later without significant rebuilding.
How long do I have to wait after a bone graft to get my dental implant? Patience is important during this stage, as we need to give your body time to build a strong, new bone foundation. For most people, the healing period is about three to four months. However, this timeline can vary depending on your individual healing process and the type of graft material used. Your specialist will monitor your progress closely to determine the perfect time to place your implant for the best long-term results.
Will I be able to feel the graft material or the membrane in my mouth while it’s healing? You shouldn’t feel the materials themselves. The bone graft is placed down inside the tooth socket, and the protective membrane is a very thin layer that sits over it, beneath your gum tissue. You might notice a feeling of fullness in the area for the first few days, but the site is designed to heal smoothly without you noticing the components working behind the scenes.
Key Takeaways
- Don’t ignore the gap—your jawbone is at risk: After a tooth is pulled, the underlying jawbone immediately begins to shrink. This process, called resorption, can affect your facial shape and your ability to get an implant later on.
- Bone grafting is the key to a strong implant foundation: Think of a bone graft as preparing the ground for a new tooth. It rebuilds the lost bone structure, creating the solid, stable base that a dental implant needs to be successful for life.
- Choose an implant to stop bone loss for good: Unlike other options, a dental implant fuses with your jaw and acts like a natural tooth root. This provides the stimulation needed to halt bone loss, protect your facial structure, and secure your smile permanently.
Related Articles
- Dental Implants In Denver • Dental & Implant Centers Of Colorado
- Do I Qualify For Implants? — Dental & Implant Centers of Colorado
- The Implant Process — Dental & Implant Centers of Colorado
- Dental Implant FAQ — Dental & Implant Centers of Colorado
- Dental & Implant Centers of Colorado — Dentist — Colorado