After your dental implant surgery, it’s normal to experience some mild discomfort and swelling. But as the days pass, you might start wondering what’s normal and what isn’t. Is the pain supposed to be getting better? Why does the area still look red? These are valid questions, and the answers often revolve around identifying a potential dental implant infection. Knowing the difference between typical healing and the signs of a problem can give you peace of mind. We’ll break down the specific symptoms to watch for, helping you understand when it’s time to relax and when you should call your dentist for a check-up.
Dental implants are a life-changing solution for many individuals, enhancing both the appearance of a smile and overall oral functionality. They provide a permanent alternative to missing teeth, restoring confidence and improving daily comfort. However, the dental implant process is invasive and often requires multiple surgical steps. While the procedure is generally successful, as with any surgery, complications can arise. One of the most common issues following implant placement is infection. Although dental implant infections are rare, proper post-surgical care is crucial to preventing complications and ensuring long-term success. Dr. Dhawan at Dental & Implant Centers Of Colorado emphasizes the importance of being well-informed about the procedure and potential risks.
How a Dental Implant Becomes Your New Tooth
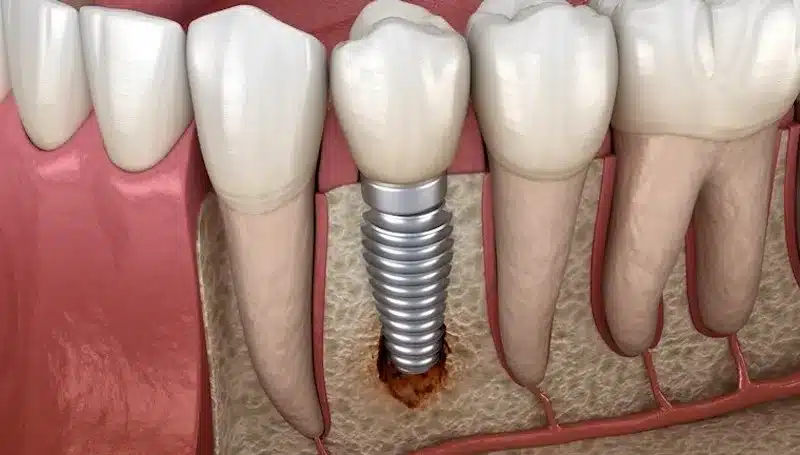
Dental implants serve as a permanent solution for missing teeth. The process begins with a dentist surgically placing a small screw-like titanium post into the jawbone. This post acts as the root of the new tooth. For patients with significant bone loss, a bone graft may be required before implant placement to ensure stability. Once the implant integrates with the bone—a process called osseointegration—it creates a strong foundation for the artificial tooth. After healing, a custom-made crown is attached to the implant, resulting in a tooth that looks, feels, and functions naturally.
What Exactly Is a Dental Implant Infection?
A dental implant infection occurs when bacteria cause inflammation around the implant site. There are two primary types of infections associated with dental implants:
Peri-implant Mucositis: An Early Warning Sign
This is a mild infection characterized by inflammation of the soft tissue surrounding the implant. It is commonly caused by poor oral hygiene and plaque buildup. At this stage, there is no significant bone loss, and the condition can often be reversed with proper care.
Peri-implantitis: A More Serious Infection
If peri-implant mucositis goes untreated, it can develop into peri-implantitis—a more severe infection that affects both soft and hard tissues around the implant. This condition can lead to significant bone loss and may compromise the stability of the implant.
How Common Are Dental Implant Infections?
Hearing the word “infection” can be unsettling, but it’s important to know that complications with dental implants are not the norm. The vast majority of procedures are successful, giving patients a new lease on life with a restored smile. However, being aware of the risks is part of being an informed patient. The more serious infection, peri-implantitis, can affect a percentage of implants over time, which is why your dentist will stress the importance of diligent aftercare. The good news is that the overall rate of significant implant infections is quite low, estimated to be around 5-10% of cases. Your outcome is greatly influenced by factors like your overall health, oral hygiene, and the skill of your surgical team. Working with an experienced specialist in dental implants helps ensure your procedure is done correctly from the start, setting you up for long-term success.
Recognizing the Signs of a Dental Implant Infection
While post-surgical healing naturally involves some discomfort, prolonged or worsening symptoms may indicate an infection. The most common signs include:
Persistent Pain or Trouble Chewing
Mild pain is expected after a dental implant procedure, but it should be manageable with pain relievers. If the pain intensifies over time or interferes with talking and chewing, it could signal an infection.
Fever, Redness, or Swelling Around the Implant
Swelling around the implant site is normal in the first few days, but if it persists or worsens, especially when accompanied by fever and redness, an infection may be developing.
A Persistent Bad Taste or Bad Breath
Bacteria buildup can result in a persistent foul taste in the mouth, often accompanied by bad breath. This is a common symptom of peri-implant infection.
Bleeding or Pus Near the Implant Site
Prolonged bleeding or pus discharge from the implant site is a serious sign of infection. Any unusual discharge should be evaluated by a dentist immediately.
Does Your Dental Implant Feel Loose?
Dental implants are designed to integrate with the jawbone and remain stable. If an implant feels loose or wobbly, it may indicate bone loss or implant failure due to infection.
Visible Implant Threads
In a healthy dental implant, the titanium post should be completely covered by your gum tissue and securely anchored in the jawbone. If you start to see the threads or ridges of the implant post becoming visible above the gumline, it’s a significant red flag. This exposure often means the surrounding gum tissue has receded, which can be a direct result of inflammation and infection. More critically, visible threads can indicate that the underlying bone supporting the implant has started to deteriorate. Think of it as the foundation of a house beginning to erode—it compromises the stability of the entire structure. Noticing this change is a clear signal to schedule a dental appointment right away.
Why Early Infections Can Be Silent
One of the trickiest things about dental implant infections, especially peri-implantitis, is that they often don’t cause pain in the early stages. You might feel perfectly fine, with no discomfort or obvious symptoms, while bacteria are quietly causing damage below the gumline. This is why you can’t rely on pain as your only indicator of a problem. Because the infection can progress silently, it can lead to significant bone loss before you even realize something is wrong. This makes regular dental check-ups absolutely essential. An experienced dentist can spot the subtle, early signs of trouble that you might miss, allowing for intervention before the implant’s stability is compromised.
How a Dentist Diagnoses an Infection
If you’re experiencing any of the symptoms mentioned or simply feel that something isn’t right with your implant, the first and most important step is to get a professional evaluation. Self-diagnosing is never a good idea, as the signs of infection can be subtle and easily mistaken for something else. A dentist has the tools and expertise to accurately identify the problem and its severity. At Dental & Implant Centers of Colorado, our expert team uses a combination of visual examination and advanced imaging to get a complete picture of your oral health and determine the best course of action for protecting your implant.
Dental Probing and Visual Checks
When you come in for an evaluation, your dentist will start with a thorough hands-on examination. This includes a careful visual check of the area around the implant, looking for signs of redness, swelling, or pus. They will also use a tool called a dental probe to gently measure the depth of the gum pockets surrounding the implant. Healthy gums fit snugly around the implant, creating shallow pockets. Deeper pockets are a sign of inflammation and gum detachment, which can indicate an infection is present. This simple, painless check provides crucial information about the health of your gum tissue and is one of the first steps in diagnosing peri-implant mucositis or peri-implantitis.
X-Rays to Assess Bone Health
While a physical exam can reveal the condition of your gums, an X-ray is essential for seeing what’s happening below the surface. X-rays allow your dentist to assess the health of your jawbone and check for any bone loss around the implant. This is the definitive way to diagnose peri-implantitis, as bone deterioration is its primary characteristic. The images clearly show the bone level, allowing your dentist to determine the extent of the damage and the stability of the implant. This diagnostic step is critical for creating an effective treatment plan to halt the infection and save your dental implant before the damage becomes irreversible.
What Causes a Dental Implant Infection?
Several factors can contribute to dental implant infections, including:
- Poor oral hygiene leading to bacterial buildup
- Smoking, which slows healing and increases infection risk
- Allergic reactions to the implant material
- Chronic health conditions such as diabetes
- A weakened immune system
- Misaligned bite, leading to excessive pressure on the implant
- Teeth grinding or clenching
- Significant bone loss in the jaw
Poor Oral Hygiene and Biofilms
Just like your natural teeth, dental implants require consistent and thorough care. If you don’t maintain good oral hygiene, bacteria can accumulate around the implant, forming a sticky film called plaque. Over time, this plaque hardens and creates a biofilm, which is a community of bacteria that can be tough to remove. This buildup is a primary cause of peri-implantitis, an infection where harmful bacteria attack the gum and bone structure supporting your implant. To prevent this, it’s essential to brush twice a day, floss daily, and attend regular check-ups. Our team can help you establish a routine and provide professional dental cleanings to keep your implant and surrounding tissues healthy for years to come.
Pre-existing Health Conditions
Your overall health plays a significant role in the success of your dental implant. Certain pre-existing conditions, especially those that affect your body’s ability to heal or fight infection, can increase your risk. For example, uncontrolled diabetes can slow down the healing process and make you more susceptible to infections around the implant site. Similarly, autoimmune disorders or other conditions that weaken the immune system can complicate recovery. That’s why a comprehensive health evaluation is a critical first step. Our expert team takes a holistic approach, carefully reviewing your medical history to ensure that a dental implant is a safe and effective option for you, creating a personalized plan that accounts for your unique health needs.
Issues During or After the Procedure
The success of a dental implant heavily relies on the skill and precision of the dental surgeon. Complications that lead to infection can sometimes arise from the procedure itself. Issues like improper placement of the implant, incorrect angling, or even a small amount of dental cement being left behind near the implant can create areas where bacteria thrive. If an infection becomes severe and the implant loosens, it might need to be removed. Choosing an experienced and highly qualified specialist is the best way to minimize these risks. At Dental & Implant Centers of Colorado, we use advanced techniques to ensure precise and successful implant placement, prioritizing your long-term health and the stability of your new tooth.
How to Prevent a Dental Implant Infection
Following proper aftercare instructions significantly reduces the risk of infection. Key preventive measures include:
Maintain Excellent Oral Hygiene
Brushing twice a day and flossing help prevent bacteria buildup around the implant site. Maintaining a clean oral environment promotes healing and prevents infections.
Rinse with a Medicated or Saltwater Mouthwash
Using a dentist-recommended mouthwash or a saltwater rinse can help reduce bacterial accumulation. Rinsing regularly is particularly important in the first few weeks after surgery.
Avoid Smoking for Better Healing
Smoking introduces harmful bacteria into the mouth and impairs healing. Patients should quit smoking before and after the implant procedure to reduce the risk of complications.
Limit Sugary Foods and Drinks
High-sugar foods and drinks encourage bacterial growth, increasing the risk of infection. Patients should minimize sugar intake during the healing process. Additionally, reducing physical activity for a few days post-surgery and taking prescribed antibiotics as directed help ensure proper healing.
Commit to Regular Dental Checkups
Your commitment to your new smile doesn’t stop after the final crown is placed. Think of your dental implant as a long-term investment in your health, and like any valuable investment, it requires consistent maintenance. Scheduling regular checkups and professional cleanings is one of the most effective ways to protect your implant. These appointments allow your dental team to monitor the implant site, check for early signs of infection like peri-implant mucositis, and ensure everything is healing correctly. Catching a potential issue early on makes treatment much simpler and significantly increases the likelihood of saving your implant. It’s a small step that makes a huge difference in the long-term success of your new tooth.
What to Do if You Suspect a Dental Implant Infection
Early intervention is crucial when dealing with dental implant infections. Ignoring symptoms can lead to worsening conditions, implant failure, and even systemic infections. If any signs of infection appear, such as persistent pain, swelling, or bleeding, patients should contact their dentist immediately for evaluation and treatment.
Treatment Options for Dental Implant Infections
If you suspect an infection, the most important step is to see your dentist right away. The good news is that several effective treatments are available, especially when the issue is caught early. Your dental team will assess the severity of the infection and recommend a course of action tailored to your specific situation. The goal is always to save the implant if possible, eliminate the infection, and restore your oral health. Treatment can range from simple, non-invasive cleaning to more involved surgical procedures. At Dental & Implant Centers of Colorado, our specialists are equipped to handle all stages of implant complications, ensuring you receive the expert care you need to get your smile back on track.
Non-Surgical Treatment
For mild infections like peri-implant mucositis, a non-surgical approach is often the first line of defense. This typically involves a professional cleaning process known as mechanical debridement, where your dentist or hygienist carefully removes plaque and calculus buildup from around the implant and surrounding gum tissue. Think of it as a targeted deep cleaning for your implant. In some cases, this cleaning is paired with a course of antibiotics to help reduce harmful bacteria and control the infection. This method is most effective when the infection is limited to the soft tissues and hasn’t caused any significant bone loss, highlighting why early detection and regular check-ups are so critical.
Surgical Treatment
When an infection progresses to peri-implantitis and causes bone loss, non-surgical methods may not be enough. In these more advanced cases, a surgical approach is often necessary to access and thoroughly clean the infected area. One common procedure is resective surgery, which involves lifting the gum tissue to remove the infected material and reshape the bone. Another option is a regenerative approach, where bone grafting materials are used to help rebuild the bone that has been lost around the implant. These advanced surgical solutions are designed to stop the infection’s progression and create a healthier environment to support the implant for the long term.
Implant Removal
In severe cases where the infection has caused extensive bone damage and the implant has become loose, removal may be the only viable option. While this can be disheartening, it’s a necessary step to completely eliminate the infection and prevent it from spreading further. Removing the compromised implant allows the site to heal properly. After a healing period, your dentist will evaluate the area to determine if the bone is healthy enough for a new implant. Often, a bone graft can be performed to prepare the site, giving you another opportunity to restore your smile with a stable, long-lasting dental implant in the future.
Complications of an Untreated Infection
Ignoring the signs of a dental implant infection can lead to serious consequences that extend beyond your mouth. What starts as a minor issue can quickly escalate, jeopardizing not only your implant but also your overall well-being. An untreated infection creates a chronic state of inflammation in your body, which can have far-reaching effects. The bacteria responsible for the infection can enter the bloodstream and travel to other parts of the body, potentially contributing to systemic health problems. This is why it’s so important to address any symptoms promptly and work with your dental team to resolve the issue before it becomes more complex and difficult to manage.
Impact on Overall Health
Locally, an untreated infection will continue to destroy the bone supporting your implant, leading to implant failure. Once an implant fails, the replacement process becomes more complicated and costly. Beyond the mouth, the chronic inflammation and bacteria from a dental implant infection can have systemic effects. Research has shown that oral infections can affect your overall health, potentially impacting conditions related to your heart and other vital organs. Treating a dental implant infection isn’t just about saving your tooth—it’s about protecting your entire body from the spread of harmful bacteria and inflammation, reinforcing the critical link between oral health and systemic wellness.
Your Next Steps for a Healthy Dental Implant
Dental implants can last a lifetime when properly cared for. However, poor oral hygiene and neglecting post-operative care can increase the risk of infection. Dr. Dhawan stresses the importance of following all aftercare instructions and consulting with a dental professional if any concerns arise. If left untreated, implant infections will not resolve on their own and can cause significant damage to oral health. Prompt action is essential for preserving dental implants. If you suspect an infection, schedule a visit to Dental & Implant Centers Of Colorado as soon as possible. At Dental & Implant Centers Of Colorado, we provide advanced dental implant solutions and comprehensive patient care to ensure long-lasting, successful results. Book your appointment today for expert dental care and guidance!
Frequently Asked Questions
Can a dental implant get infected years after it was placed? Yes, an infection can develop at any time, even years after your implant has fully healed. Late-stage infections are often linked to changes in oral hygiene, the development of other health conditions, or lifestyle factors like smoking. This is precisely why your long-term commitment to regular dental check-ups is so crucial for protecting your investment and ensuring your implant lasts a lifetime.
If my implant doesn’t hurt, does that mean it’s not infected? Not necessarily. One of the trickiest things about implant infections is that they can be completely painless in their early stages. You might not feel any discomfort while bacteria are quietly causing inflammation and bone loss below the gumline. This is why you can’t rely on pain as your only warning sign. Regular exams and X-rays are the best tools for catching these silent problems early.
How can I tell the difference between normal healing and an infection right after surgery? After your procedure, you should expect some mild discomfort, swelling, and maybe even a little bruising for a few days. The key is that these symptoms should gradually improve each day. An infection, on the other hand, tends to get worse. If you notice pain that intensifies instead of fading, or swelling that returns after it had started to go down, that’s a sign to call your dentist.
Should I take antibiotics before my regular dental cleanings to prevent an infection? For the vast majority of patients, taking antibiotics before a routine cleaning is not necessary. Prophylactic antibiotics are typically only recommended for individuals with specific medical conditions, such as certain heart problems or a compromised immune system. This is a decision that should be made by your dentist and physician based on your unique health history, not a standard practice for everyone with an implant.
What should I do if I notice a sign of infection over the weekend? If you’re experiencing severe symptoms like intense pain, significant swelling that affects your ability to open your mouth, or a fever, you should seek immediate attention. Most dental practices have an after-hours number for true emergencies. For less severe signs, like minor bleeding when you brush or persistent bad breath, make a note of it and call your dentist’s office first thing Monday morning to schedule an appointment.
Key Takeaways
- Pain Isn’t the Only Red Flag: An infection can develop without causing discomfort, so watch for other signs like persistent swelling, redness, a bad taste, or a loose-feeling implant. Noticing these subtle changes early is key.
- Your Daily Habits Are Your Best Defense: Consistent brushing and flossing are non-negotiable for preventing the bacterial buildup that leads to infection. Pairing your at-home care with regular professional cleanings ensures your implant stays healthy for the long haul.
- When in Doubt, Reach Out: If you suspect something is wrong with your implant, don’t wait it out. A quick call to your dentist for an evaluation can lead to a simple fix and prevent more complex issues, like bone loss or implant failure.
Related Articles
- Dental Implant FAQ — Dental & Implant Centers of Colorado
- Do I Qualify For Implants? — Dental & Implant Centers of Colorado
- The Implant Process — Dental & Implant Centers of Colorado
- Single Dental Implants — Dental & Implant Centers of Colorado
- Dental & Implant Centers of Colorado — Dentist — Colorado